Services
Work Injuries
When a patient visits their chiropractor due to a work injury, the chiropractor routinely looks beyond the actual injury and addresses concern towards their station setup, whether they use ergonomically correct equipment, and whether they utilize proper work techniques. The goal is both to help relieve your pain and determine how to avoid what caused it in the first place. Work injuries can occur in a variety of different work environments including construction sites, offices, warehouses, and retail stores. Much of the time, the causes of pain in the workplace include:
- Falls caused by Overexertion
- Improper lifting
- Repetitive strain
- Blunt force trauma
- Exposure to Chemicals
- Burns
Most workplace injuries are the result of soft tissue and joint damage. Improper lifting techniques are one of the most common reasons for the occurrences of pain in the workplace. You may consider visiting a chiropractor if you are experiencing any of the following pains due to your workplace injuries or otherwise:
- Back injuries (sprains, strains, disc problems)
- Neck injuries (sprains, strains, joint dysfunction)
- Carpal tunnel syndrome
- Headache (caused by muscle tension, joint dysfunction, or poor posture)
- Numbness and tingling of extremities.
Whiplash
Describing a range of injuries to the neck caused by or related to a sudden distortion of the neck. Cervical acceleration-deceleration” (CAD) describes the mechanism of the injury, while the term “whiplash associated disorders” (WAD) describes the injury and symptoms.
Anatomy
There are four phases that occur during “whiplash”:
- Initial position (before the collision),
- retraction
- extension
- rebound
In the initial position, there is no force on the neck due to inertia keeping it stable. Anterior longitudinal ligament injuries in whiplash may lead to cervical instability. They explain that during the retraction phase, that is when the actual “whiplash” occurs, since there is an unusual loading of soft tissues. The next phase is the extension, the whole neck and head switch to extension, and it is stopped or limited by the head restraint. The rebound phase transpires as a result of the phases that are mentioned.
During the refraction phase the spine forms an S-Shaped curve, and this caused by the flexion in the upper planes and hyperextension at the lower planes and this exceed their physiological limits this phase the injuries occur to the lower cervical vertebrae. At the extension phase all cervical vertebrae and the head are fully extended, but do not surpass their physiological limits. Most of the injuries happen in C-5 and C-6.
Symptoms
Symptoms reported by sufferers include pain and aching to the neck and back, referred pain to the shoulders, sensory disturbance (such as pins and needles) to the arms and legs, and headaches. Symptoms can appear directly after the injury but often are not felt until days afterward. Whiplash is usually confined to the spine. The most common areas of the spine affected by whiplash are the neck and middle of the spine. “Neck” pain is very common between the shoulder and the neck.
Sports Injuries
Sports injuries are injuries that occur in athletic activities. They can result from acute trauma, or from overuse of a particular body part.
Classification
Traumatic injuries account for most injuries in contact sports such as Ice Hockey, Association football, rugby league, rugby union, Australian rules football, Gaelic football and American football because of the dynamic and high collision nature of these sports.[citation needed] Collisions with the ground, objects, and other players are common, and unexpected dynamic forces on limbs and joints can cause injury.
Traumatic injuries can include:
- Contusion or bruise – damage to small blood vessels which causes bleeding within the tissues.
- Strain – trauma to a muscle due to overstretching and tearing of muscle fibers
- Sprain – an injury in a joint, caused by the ligament being stretched beyond its own capacity
- Wound – abrasion or puncture of the skin
- Bone fracture
- Head injury
- Spinal cord injury
In sports medicine, a catastrophic injury is defined as severe trauma to the human head, spine, or brain.
Concussions in sport became a major issue in the United States in the 2000s, as evidence connected repeated concussions with chronic traumatic encephalopathy and increased suicide risk.
Overuse and repetitive stress injury problems associated with sports include:
- Runner’s knee
- Tennis elbow
- Tendinosis
Some activities have particular risks:
- Bicycle safety
- Gun safety
- Sailing ship accidents
- Skateboarding
Soft tissue injuries
When soft tissue experiences trauma, the dead and damaged cells release chemicals, which initiate an inflammatory response. Inflammation is characterized by pain, localized swelling, heat, redness and a loss of function. Small blood vessels are damaged and opened up, producing bleeding within the tissue. In the body’s normal reaction, a small blood clot is formed in order to stop this bleeding and from this clot special cells (called fibroblasts) begin the healing process by laying down scar tissue.
The inflammatory stage is therefore the first phase of healing. However, too much of an inflammatory response in the early stage can mean that the healing process takes longer and a return to activity is delayed. Sports injury treatments are intended to minimize the inflammatory phase of an injury, so that the overall healing process is accelerated. Intrinsic and extrinsic factors are determinant for the healing process.
Treatment
Sports injuries can be treated and managed by using the P.R.I.C.E.S… DR. ABC, and T.O.T.A.P.S regimes:
| P – Protect R – Rest I – Ice C – Compression E – Elevation S – Stabilize | D – Danger R – Response | A – Airway B – Breathing C – Circulation | T – Talk O – Observe T – Touch A – Active movement P – Passive movement S – Skills test |
The primary inflammatory stage typically lasts around 5 days and all treatment during this time is designed to address the cardinal signs of inflammation – pain, swelling, redness, heat, and a loss of function. Compression sportswear is becoming very popular with both professional and amateur athletes. These garments are thought to both reduce the risk of muscle injury and speed up muscle recovery.
Sleep Apnea
Each pause in breathing is called an apnea. Sleep apnea is sleeping disorder that consists of pauses in an apnea can last anywhere from ten seconds to several minutes. In sufferers of sleep apnea, this can occur 5 to 30 times per hour or more, causing shallow and/or infrequent breathing during sleep.
There are three forms of sleep apnea: central (CSA), obstructive (OSA), and complex or mixed sleep apnea. In CSA, the disorder is characterized by lack of respiratory effort, in OSA breathing is interrupted by a physical blocking of airflow despite the respiratory effort. Suffers of the condition may start to experience sleepiness or fatigue due to their symptoms and level of sleep disturbance. Both adults and children can suffer from sleep apnea
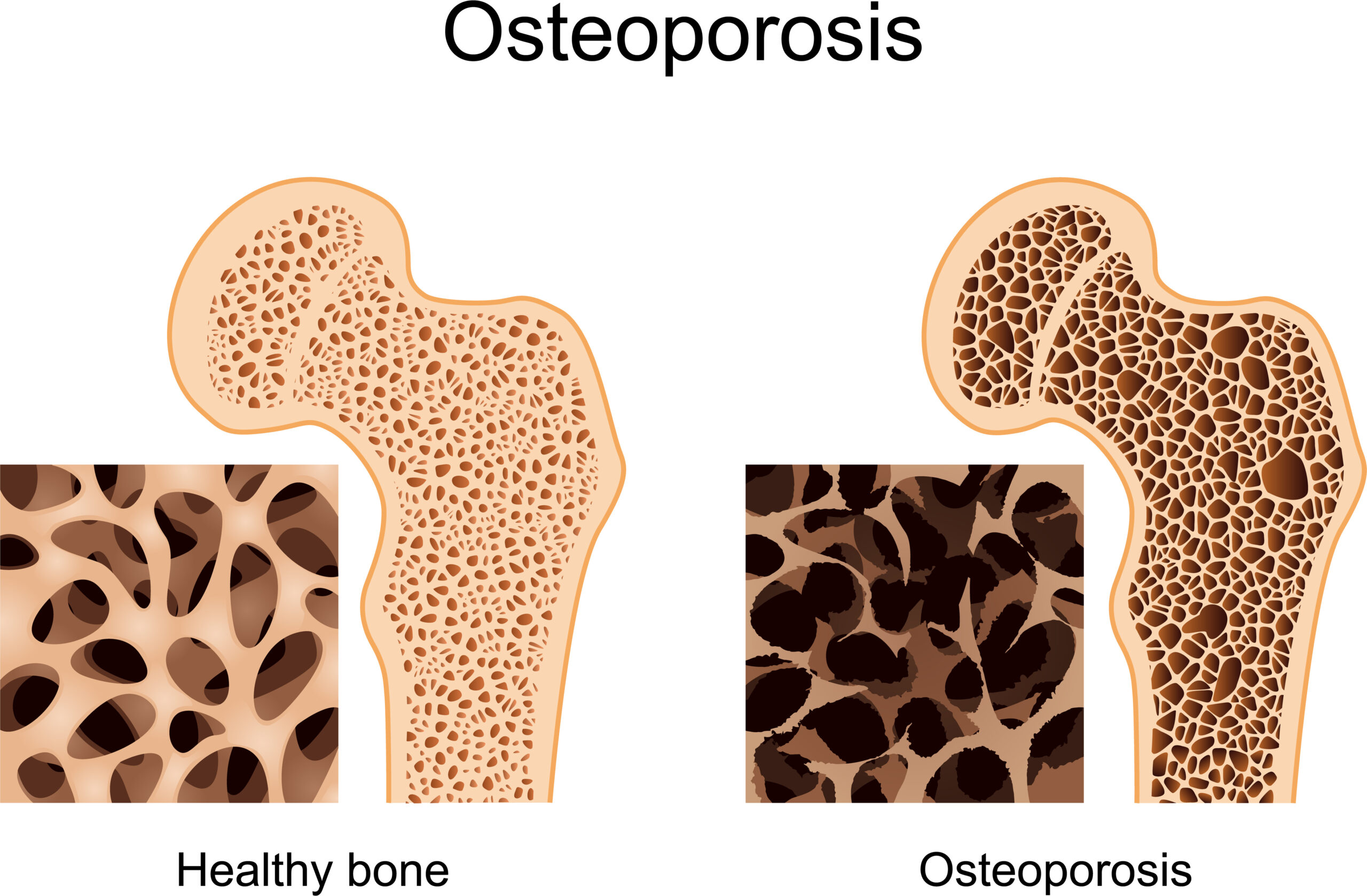
Osteoporosis
Osteoporosis is a progressive bone disease that is characterized by a decrease in bone mass and density and that leads to an increased risk of fracture. In osteoporosis, the bone mineral density (BMD) is reduced, bone microarchitecture deteriorates, and the amount and variety of proteins in bone are altered.
Osteoporosis is defined by the World Health Organization (WHO) as a bone mineral density of 2.5 standard deviations or more below the mean peak bone mass (average of young, healthy adults) as measured by dual-energy X-ray absorptiometry; the term “established osteoporosis” includes the presence of a fragility fracture. The disease may be classified as primary type 1, primary type 2, or secondary.
The form of osteoporosis most common in women after menopause is referred to as primary type 1 or postmenopausal osteoporosis. Primary type 2 osteoporosis or senile osteoporosis occurs after age 75 and is seen in both females and males at a ratio of 2:1. Secondary osteoporosis may arise at any age and affect men and women equally. This form results from chronic predisposing medical problems or disease, or prolonged use of medications such as glucocorticoids, when the disease is called steroid- or glucocorticoid-induced osteoporosis.
The risk of osteoporosis fractures can be reduced with lifestyle changes and in those with previous osteoporosis related fractures medications. Lifestyle change includes diet, exercise, and preventing falls. The utility of calcium and vitamin D is questionable in most. Bisphosphonates are useful in those with previous fractures from osteoporosis but are of minimal benefit in those who have osteoporosis but no previous fractures. Osteoporosis is a component of the frailty syndrome.
Risk Factors
- Excess alcohol: Although small amounts of alcohol are probably beneficial (bone density increases with increasing alcohol intake), chronic heavy drinking (alcohol intake greater than three units/day) probably increases fracture risk despite any beneficial effects on bone density.
- Vitamin D deficiency: Low circulating Vitamin D is common among the elderly worldwide. Mild vitamin D insufficiency is associated with increased parathyroid hormone (PTH) production. PTH increases bone resorption, leading to bone loss. A positive association exists between serum 1,25-dihydroxycholecalciferol levels and bone mineral density, while PTH is negatively associated with bone mineral density.
- Tobacco smoking: Many studies have associated smoking with decreased bone health, but the mechanisms are unclear. Tobacco smoking has been proposed to inhibit the activity of osteoblasts and is an independent risk factor for osteoporosis. Smoking also results in increased breakdown of exogenous estrogen, lower body weight, and earlier menopause, all of which contribute to lower bone mineral density.
- Malnutrition: Nutrition has an important and complex role in the maintenance of good bone health. Identified risk factors include low dietary calcium and/or phosphorus, magnesium, zinc, boron, iron, fluoride, copper, vitamins A, K, E, and C (and D where skin exposure to sunlight provides an inadequate supply). Excess sodium is a risk factor. High blood acidity may be diet-related and is a known antagonist of bones. Some have identified low protein intake as associated with lower peak bone mass during adolescence and lower bone mineral density in elderly populations. Conversely, some have identified low protein intake as a positive factor, protein is among the causes of dietary acidity. The imbalance of omega-6 to omega-3 polyunsaturated fats is yet another identified risk factor.
- Underweight/inactive: Bone remodeling occurs in response to physical stress, so physical inactivity can lead to significant bone loss. Weight-bearing exercise can increase peak bone mass achieved in adolescence, and a highly significant correlation between bone strength and muscle strength has been determined. The incidence of osteoporosis is lower in overweight people.
- Heavy metals: A strong association between cadmium and lead with bone disease has been established. Low-level exposure to cadmium is associated with an increased loss of bone mineral density readily in both genders, leading to pain and increased risk of fractures, especially in the elderly and in females. Higher cadmium exposure results in osteomalacia (softening of the bone).
- Soft drinks: Some studies indicate soft drinks (many of which contain phosphoric acid) may increase the risk of osteoporosis, at least in women. Others suggest soft drinks may displace calcium-containing drinks from the diet rather than directly causing osteoporosis.
Neck Pain
Neck pain, although felt in the neck, can be caused by numerous other spinal problems. Neck pain may arise due to muscular tightness in both the neck and upper back, or pinching of the nerves emanating from the cervical vertebrae. Joint disruption in the neck creates pain, as does joint disruption in the upper back. Two thirds of the population will suffer from neck pain at some point in their lives.
The most common causes of neck pain include:
- Stress
- Prolonged postures
- Minor injuries and falls
- Referred pain
- Over-use
- Whiplash
- Herniated disc
- Pinched nerve
Massage Therapy
Massage is the manipulation of superficial and deeper layers of muscle and connective tissue using various techniques, to enhance function, aid in the healing process, decrease muscle reflex activity, inhibit motor-neuron excitability, promote relaxation and well-being, and as a recreational activity.
Evidence strongly suggests early mobilization and range of motion exercises greatly improve recovery from nearly any injury or surgery.
Therapeutic Massage is used to:
- Reduce headache-related symptoms including migraines
- Reduce blood pressure
- Reduce stress
- Reduce depression
- Reduce Anxiety
- Reduce Allergies
- Reduce Allergies
- Improve circulation
- Increase muscle elasticity
- Treat sport injuries
- Increase muscle tone, and flexibility
- Allergies
- Relax
Leg Pain
The sciatic nerve is the largest nerve in the human body and one of the most common causes of leg pain. The term sciatica is used to describe the symptoms of pain occurring in the leg and lower back. Some use the term specifically to mean a nerve dysfunction caused by compression of one or more lumbar or sacral nerve roots from a spinal disc herniation.
When the liquid center of a disc bulges outwards, herniation occurs. The bulged disc can then tear against external ring fibers, contact the spinal canal, and compress a nerve root against the lamina or pedicle of a vertebra. This causes sciatica. The liquid extruded when this happens can cause inflammation and swelling of the surrounding tissue which can further compress the nerve root into the confined space of the spinal canal.
Sciatic pain typically runs through the lower back and down the sciatic nerve through the leg and can even run all the way down to the foot. Numbness, tingling, burning, and pricking sensations are all symptoms that may occur in cases of sciatic injury.
Sciatica is caused by compression of lumbar nerves, sacral nerves, and/or the sciatic nerve. Sciatic damage can be permanent, thus it is important that you seek medical attention if you are suffering from these symptoms.
Joint Disorders
Fact joints are what guide and limit the movement of the spine. These joints are located in pairs on each segment of the spinal cord except for the very top of your vertebrae. Roughly one-fifth of the twisting ability of your neck and lower back is controlled by facet joints.
A small capsule surrounds each facet joint providing a nourishing lubricant for the joint. Each joint is supplied with tiny nerve fibers that provide a painful stimulus when the joint is injured or irritated. These joints can degenerate over time due to aging or disease, which can result in numerous conditions of pain.
Damage to the lower back may cause stiffness resulting in difficulty standing up or maintaining good posture. Cervical damage (near the neck) can make it difficult to move and twist your head.
When the cartilage in joints wears thin, the body begins to produce a material to shore the cartilage (these are called bone spurs). This material can calcify, hardening and causing stiffness in the joint. This can lead to inflammation and osteoporosis. Powerful muscle spasms can occur due to the inflammation. The joints can also degenerate and slip forward in a advanced cases such as spondylolisthesis.
Sacroiliac joint dysfunction, a common joint disorder, refers to pain in the sacroiliac joint region that is caused by abnormal motion in the sacroiliac joint (around your hip). This can result in debilitating pain due to inflammation of the sacroiliac joint. Common symptoms include lower back pain, buttocks pain, sciatic leg pain, groin pain, hip pain, urinary frequency, numbness, prickling, or tingling. The pain can range from dull to stabbing pain and increases with motion.
Ice Therapy
The application of ice is an excellent way to reduce inflammation and temporary pain. Ice causes constriction in the veins of the affected tissue, limiting blood flow and acting as an anesthetic. Once the ice is removed, blood will rush back to the affected area providing nutrients that will help with the healing process.
Ice therapy is often used in the treatment of back and neck pain. It lessens the severity of muscle spasms, reduces pain by causing numbness, and aids in lessening soft tissue damage.
Ice or ice packs should be wrapped in a towel while being used for treatment. Ice therapy should be used on the affected area for 24 to 48 hours from the initial ache or injury. It is recommended to reapply it every 10 minutes for maximum affect and to not leave it on for more than 20 minutes at a time.
Patients suffering from rheumatoid arthritis, Raynaud’s Syndrome, colds or allergic conditions, paralysis, or areas of impaired sensation should not use ice therapy.